Fewer Denials. Faster Payments. Greater Revenue.
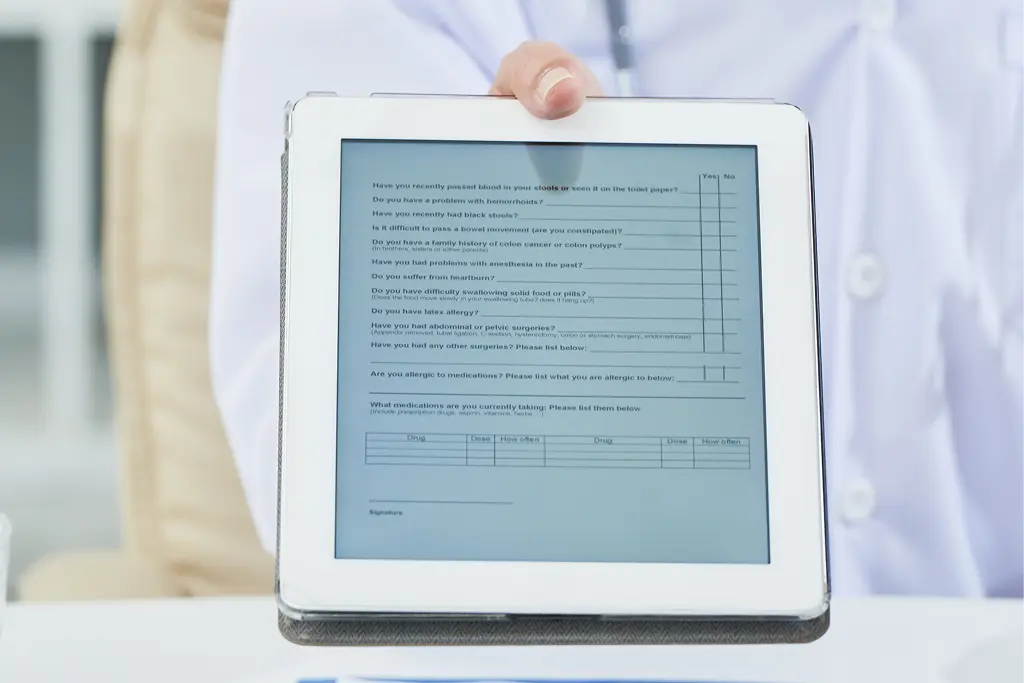
At MedicLogs, we understand that accurate patient eligibility and benefits verification is the foundation of a strong revenue cycle. Verifying insurance coverage before services are rendered helps prevent claim denials, reduce payment delays, and ensure providers are reimbursed accurately and on time.
Why Eligibility & Benefits Verification Matters
Patient eligibility verification is a critical step in the healthcare revenue cycle. Real-time access to insurance data ensures that coverage, benefits, and authorization requirements are confirmed upfront—eliminating unnecessary billing errors and administrative challenges.
A reliable verification process leads to cleaner claims, fewer rejections, and smoother revenue flow.

Key Benefits of Eligibility Verification
- Real-Time Accuracy: Confirm active coverage, benefits, deductibles, and copays before the visit.
- Fewer Claim Denials: Reduce rework and payment delays by eliminating eligibility-related errors upfront.
- Medicaid Eligibility Checks: Identify patients eligible for Medicaid and support proper filing to recover care costs.
- Streamlined Operations: Standardized workflows reduce staff workload and speed up the billing process.
Why Outsource Eligibility Verification to MedicLogs?
Managing eligibility checks in-house can be time-consuming and prone to errors. MedicLogs uses proven processes and payer communication to deliver accurate, timely verifications—so your team can focus on patient care, not insurance follow-ups.
What Sets MedicLogs Apart
- HIPAA-Compliant Systems: Secure handling of patient data at every step.
- Fast Turnaround Times: Verifications completed ahead of scheduled appointments.
- Error-Focused Accuracy: Detail-oriented checks to minimize eligibility-based denials.
- Cost-Effective Solutions: Reduce overhead while maintaining high accuracy.
- Revenue Optimization: Improve collections by preventing coverage-related rejections.

What Our Customers Say?

Sarah Aviva Rosner, MD

Olumuyiwa Gay MD, MPH, FAPA

